Practice Based Research Network (PBRN)
Practice Based Research Network (PBRN)
Mission: to support research among researchers, clinics, clinicians, and community partners that is collaborative and meaningful to all stakeholders.
What is a PBRN?
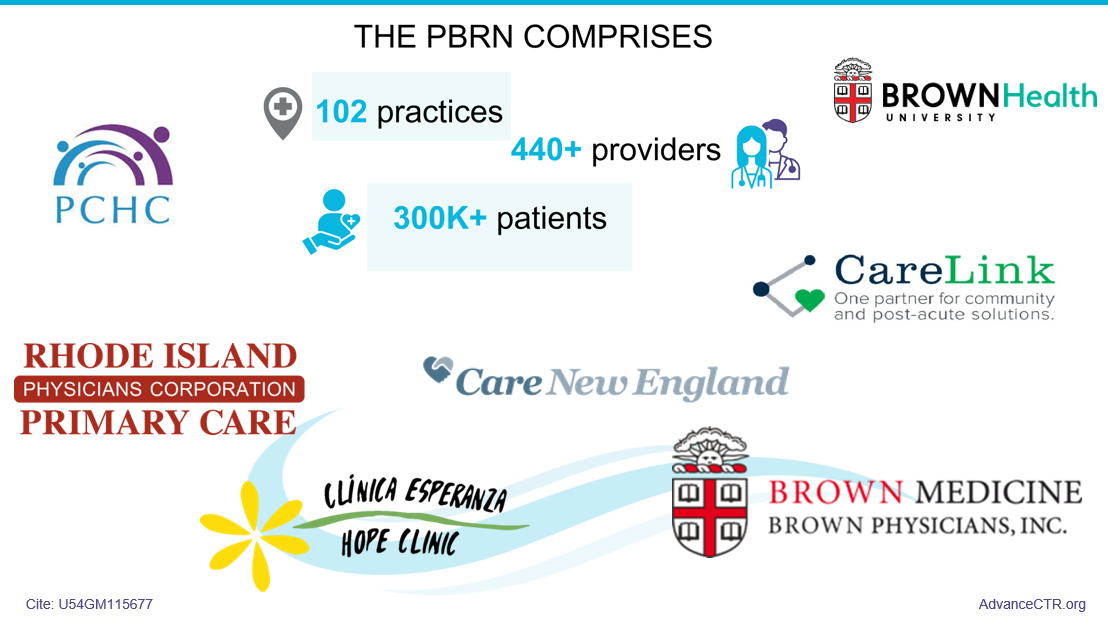
Practice-based research networks (PBRNs) are collaborations that involve practicing clinicians in formulating and answering clinical and organizational questions relevant to their practices and the communities they serve. By participation in PBRN, practice organizations and providers can access resources from Advance RI-CTR, including vetted research proposals. These proposals align with the practices and providers’ goals and priorities such as improving health care quality, fostering innovation, and achieving significant breakthroughs for patients, providers, and communities. Individual providers and practices have the flexibility to choose whether to participate in the proposed projects that have been proposed by external researchers or internally developed by the practices and/or providers.
Advance RI-CTR puts the community voice at the center of all PBRN activities. We bring community to the forefront through our Community Advisory and Action Board (CAAB) and our Community Engagement Studios. View the PBRN Operating Policies to get a sense of how it works.
Submit a Study Application Submit a Practice Application
| CURRENT PRACTICE BASED RESEARCH NETWORK (PBRN) PROJECTS | |||
| Project Name | Project PI | Project Description | Funding Source |
| Diabetes Health Equity Project | Dr. Joanne Wilkinson | Diabetes Health Equity Project is a preliminary project to further investigate disparities in diabetes outcomes in the PBRN (prior work indicated poorer outcomes with Latinx patients on some indicators). The project is a combination of 1) community-building with Progreso Latino to prepare for a community-engaged project to address disparities; 2) a secondary data analysis of PBRN data focused on the uptake of newer diabetes therapies (CGMs, GLP-1s, and low-carb diets) in Latinx patients; and 3) a systematic review of CGM use in primary care. | Advance RI-CTR |
| Patient Engagement in Diabetes Management in Urban Latinx Communities | Dr. Joanne Wilkinson | Patient Engagement in Diabetes Management in Urban Latinx Communities is a mixed methods project (survey + qualitative interviews) to investigate and describe barriers and facilitators to the newer diabetes therapies (noted above) in Latinx patients recruited through Progreso Latino's food pantry. The work-product from this project will inform the development of mixed-media interventions targeted at urban Latinx patients, likely disseminated via social media, to be developed and tested with a future proposal. | Advance RI-CTR |
| Association between Social Drivers and Cancer Screening Uptake | Dr. Joseph Diaz and Charles Eaton | Disparities in breast and colorectal cancer screening persist among under resourced communities despite standardized guidelines. This study aims to examine the association between Social Drivers of Health (SDoH) and breast and colorectal cancer screening rates in Rhode Island. Using SDoH data collected from patients within a primary care network, this study investigates the impact of factors such as housing insecurity, social isolation, and transportation difficulties on screening completion. | Internal Funding at CNE |
| Enhancing Depression Screening for Spanish-Speaking Adults in Primary Care Settings: An Implementation Science Approach | Dr. Linda E. Guzman & Dr. Hannah E. Frank | Latino adults in the U.S. face significant disparities in treatment for major depressive disorder (MDD), particularly those with limited English proficiency. Only 10% of Spanish-speaking Latinos receive treatment compared to 33% of their English-speaking counterparts. Despite primary care providers (PCPs) managing 60% of MDD cases, the Spanish-language Patient Health Questionnaire-9 (PHQ-9) is used far less frequently than the English version. Language-concordant screening is crucial to improve timely detection, treatment, and referrals. This R34 proposal, led by MPI Dr. Linda E. Guzman and Dr. Hannah E. Frank from the Brown Research on Implementation and Dissemination to Guide Evidence Use (BRIDGE) Program in the Department of Psychiatry and Human Behavior at the Warren Alpert Medical School of Brown University, aims to develop and pilot an implementation blueprint to enhance depression screening for Spanish-speaking adults. The study will be co-developed with community partners and evaluated using implementation science methods. Dr. Guzman, a bilingual clinical psychologist with extensive training in primary care behavioral health, and Dr. Frank, Associate Director of the BRIDGE Program, will conduct the study in three Rhode Island clinics where up to 70% of patients are Spanish-speaking. The results will lay the groundwork for a larger R01 project to expand the implementation of language-concordant depression screening nationwide, improving accessibility and equity in mental health care for individuals with limited English proficiency. | Working on an R34 Proposal |
| Diabetes Health Equity Data Pilot | Charles B Eaton MD,MS | Diabetes Mellitus is a common disease with high rates of mortality and morbidity that can be reduced by optimal medical care. Over 90% of routine diabetes care is performed in primary care and has been shown to have disparate outcomes based upon race, socioeconomic status, preferred language. This study will evaluate whether recommended medical management such as measurement of glucose control by hemoglobin A1c, having a hemoglobin A1c at an optimal level, evaluation of kidney function and proteinuria, control of blood pressure, medications to protect kidneys, and lower cholesterol differs by race/ethnicity, preferred language and social vulnerability index based upon zip code. This data will be presented to providers at each of the practices to plan improvements in outcomes and to the larger community effected by the health disparities to move towards health equity. | Internal Funding at CNE |